
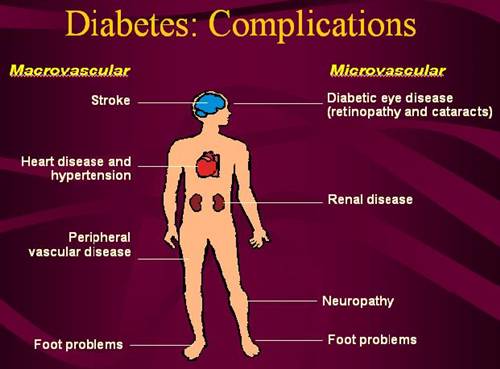
It’s a central tenet of diabetes treatment: monitor the blood sugar closely, then adjust your diet, exercise, and medications to keep it in a good range. And that makes sense. Poorly controlled blood sugar is a major risk factor for diabetic complications, including kidney disease, vision loss, and nerve damage.
While efforts to carefully monitor and control the blood sugar in diabetes are worthwhile, “tight control” is not always helpful — and it may even cause harm. For example, in studies of people with longstanding type 2 diabetes, the type that usually begins in adulthood and is highly linked with obesity, those with the tightest control either had no benefit or had higher rates of cardiovascular disease and death. Meanwhile, studies of people with type 1 diabetes — the type that tends to start during childhood due to an immune attack against the insulin-producing cells in the pancreas — suggest that tight control may help protect against cardiovascular disease. So, it seems the benefits and risks of tight control depend on the situation.
Home blood sugar monitoring for type 2 diabetes
People with diabetes are often advised to check their blood sugar levels at home by pricking a finger and testing the blood with a glucose meter. They can review the results with their doctors over the phone, online, or at the next office appointment. The value of this for people with type 2 diabetes is uncertain.

In a study published in JAMA Internal Medicine, researchers enrolled 450 people with Type 2 diabetes, none of whom were taking insulin. They were randomly assigned to one of three groups:
- No self-monitoring of blood sugar
- Once daily self-monitoring of blood sugar
- Once-daily self-monitoring of blood sugar with “enhanced feedback” from their blood glucose meters with messages intended to educate and motivate the study volunteers.
After one year these researchers found that, compared with those not self-monitoring blood sugar, those who self-monitored had no improvement in the control of their blood sugar, and had no improvement in measures of quality of life.
So what?
The impact of this study could be enormous. Of the enrolled study subjects, three-quarters routinely checked blood sugar at home. If that’s typical of people with type 2 diabetes, these findings could allow thousands of people to stop sticking themselves and save money on monitoring equipment, with no ill effects on their health.
But even if these findings are confirmed, there may be situations when home monitoring is still useful and important. For example, home monitoring might be a good idea when people like those in this study:
- Develop an infection
- Change the dose of their diabetes medications
- Add or stop taking one of their medications
- Gain or lose a significant amount of weight
- Begin taking insulin.
This study did not examine these situations and so could not draw conclusions about them. It’s also worth noting this study lasted only one year. It may take longer to see a benefit from home monitoring. Finally, this study did not include individuals with type 1 diabetes, so the results do not apply to them.
The bottom line
This new study suggests that doctors treating people with type 2 diabetes may not need to recommend routine self-monitoring of blood sugar. However, while that may be true for the average person with type 2 diabetes who is not taking insulin, we’ll need more studies and longer-term studies to identify which people with type 2 diabetes will benefit most from home monitoring and when it’s just not worth the effort.
Source :- Health Harvard

Leave a Reply